Associations of the Fibrosis-4 Index With Rates of Cardiac Events and Liver Decompensation, and the Potential Implications on Risk Stratification in Patients With Nonalcoholic Steatohepatitis.
September 23 2023
Background and aims: The non-invasive Fibrosis-4 index (FIB-4) predicts liver fibrosis and cirrhosis in patients. FIB-4 as the primary metric for risk stratification in non-alcoholic steatohepatitis (NASH) presents several critical limitations, notably regarding the risk of cardiovascular (CV) events. Recent studies highlight the FIB-4’s potential in forecasting cardiac events, however it is critical to note that FIB-4 cutoffs as currently applied may not precisely represent the risk for these outcomes. This study aims to examine association between CV events and FIB-4 score.
Method: Our study cohort comprised 1, 828 biopsy-confirmed NASH patients extracted from a deidentified, privacy-preserving database consisting of digital electronic health records (EHR) from approximately 7 million patients seen at sites over five different states from 1991 through 2020. Patients with coexisting conditions, such as hepatocellular carcinoma, alcoholism, elevated HgA1c >9% or ALT >250 U/L, viral encephalitis, bariatric surgery, and autoimmune disease, were excluded to maintain a clear focus on NASH-specific outcomes. The identification and selection of eligible patients employed a hybrid approach beginning with structured ICD diagnosis that was then enriched by natural language processing algorithms.
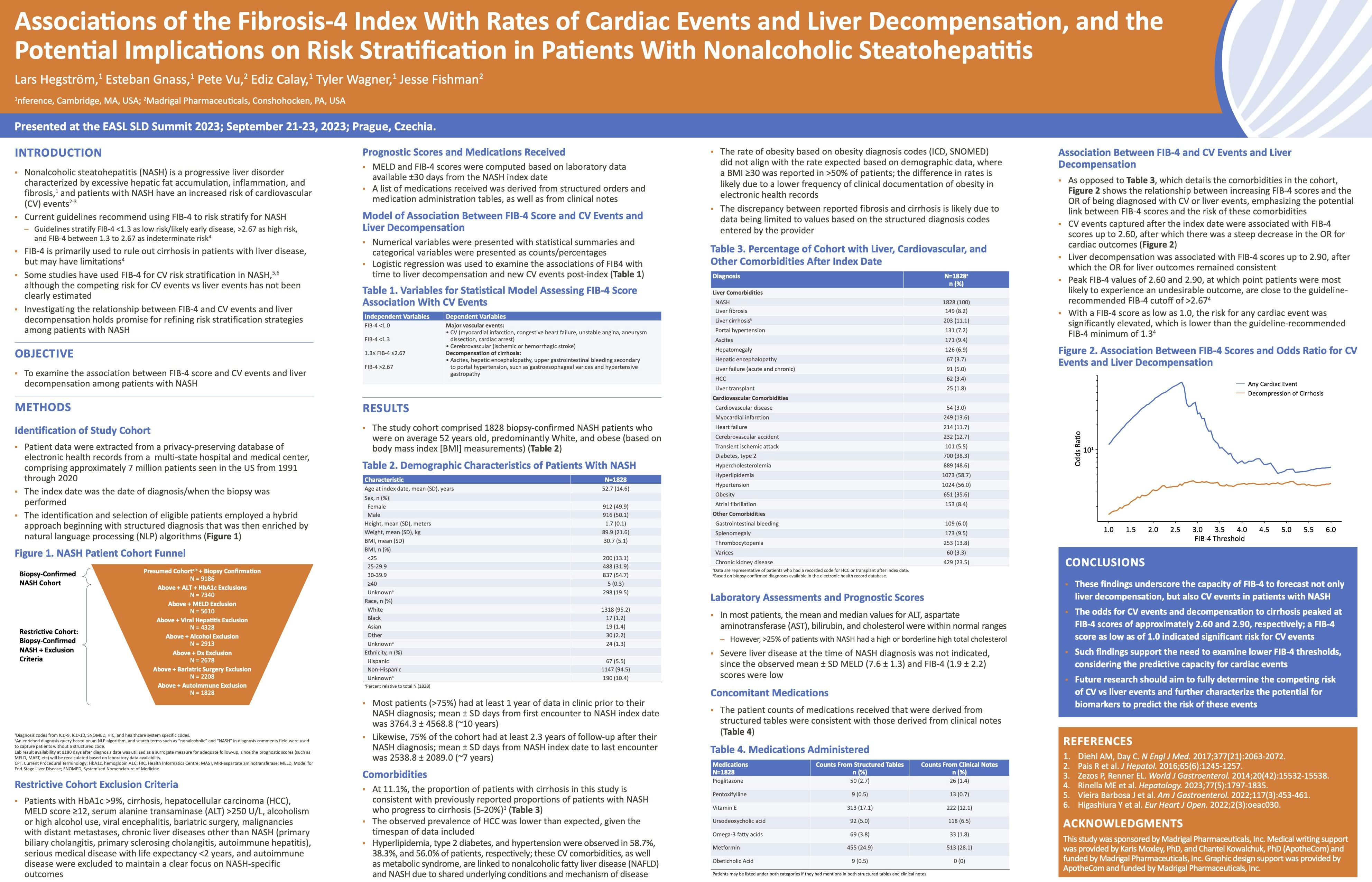
Results: Analysis revealed patterns in the relationship between FIB-4 scores and the odds ratios of liver decompensation and CV events (myocardial infarction, congestive heart failure, unstable angina, cardiac arrest, and aneurysm dissection). For CV outcomes, the odds ratio is associated with a FIB-4 score up to 2.60, and up to 2.90 for liver decompensation. The peak FIB-4 values of 2.60 and 2.90, at which point patients are most likely to experience an undesirable outcome, are close to the guideline-recommended FIB-4 cutoff of >2.67. We observed a steep decrease in the odds ratio for cardiac outcomes at FIB-4 >2.60, while the odds ratio for liver outcomes remained steady, reinforcing a shift in the relative incidences of outcomes experienced by patients with advanced liver disease. Of note with a FIB-4 score as low as 1.0, the risk for any cardiac event is significantly elevated. This is lower than the guideline-recommended FIB-4 minimum of 1.3.
Conclusion: These findings underscore the capacity of FIB-4 to forecast not only liver decompensation but also CV events in patients with NASH. The peak odds for CV events is approximately 2.60, and 2.90 for decompensation to cirrhosis, with significant risk for CV events as low as FIB-4 score of 1.0. Such findings support the need to stratify patients with an elevated FIB-4 as high-risk and also underline the critical need to revisit the lower thresholds of FIB-4 scores, now in light of considering the predictive capacity for cardiac events.